Last month we covered a bit of pathophysiology, presenting pathophysiology, presenting clinical signs and the radiographic diagnosis of gastric dilatation-volvulus (GDV).
Now we cover the three things you need to do as soon as a suspected case is presented:
- IV fluid resuscitation
- decompression of the stomach
- pain relief
Depending on the number of staff you have, all of these can be performed simultaneously. If not, follow the above order as shock is the most imminent problem.
Catheter placement
Fluid resuscitation is relatively straightforward. Most GDV patients will be in some degree of shock, varying from mild to severe. Regardless of the actual degree, all patients will require IV fluids.
The placement of IV catheters is particularly important; their numbers and diameter will influence the rate of response to treatment. Large-bore catheters allow faster flow of fluids compared to smaller ones, while multiple catheters allow concurrent delivery of two bags of fluids as opposed to one – particularly important in large dogs. Therefore, always try to place the largest catheter possible (for example, 18G or larger for large-breed dogs) into the cephalic veins.
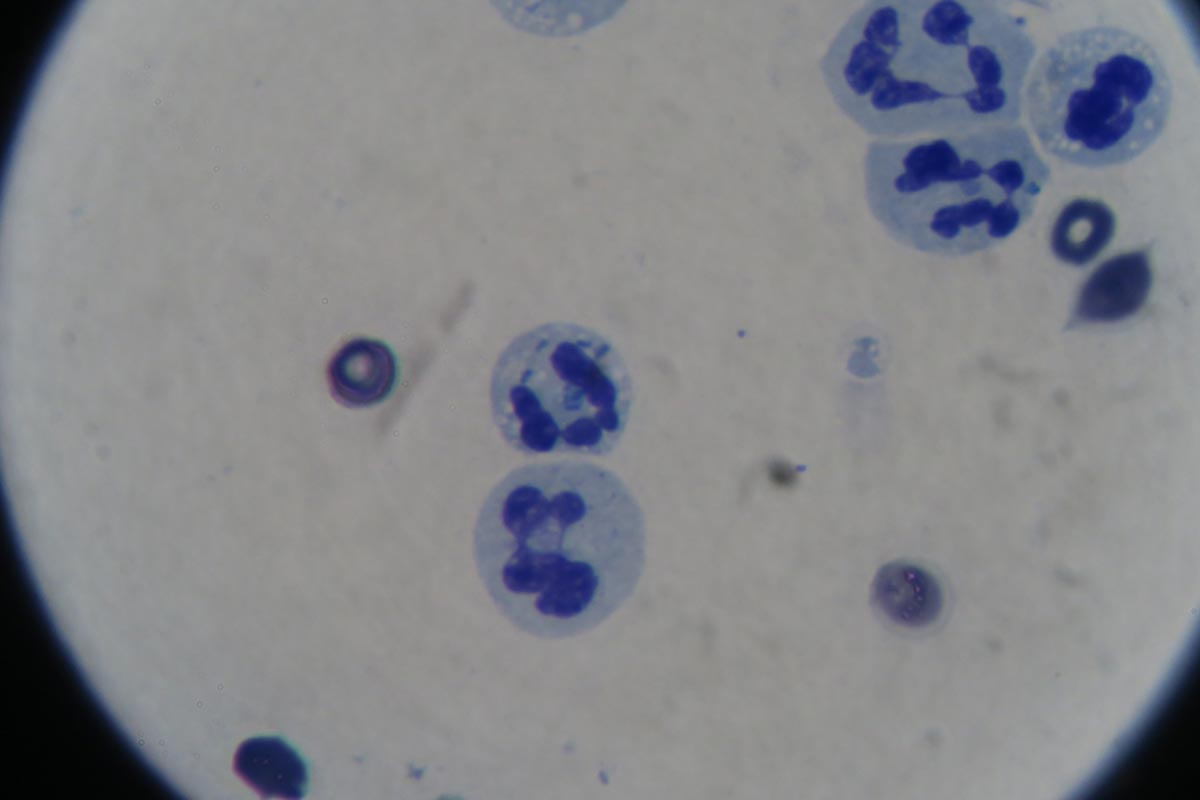
Once the catheters have been placed, collect 2ml to 3ml of blood for baseline measurements. These can be collected directly from the catheters and should include:
- PCV/total protein
- blood gas analysis
- lactate
- activated clotting time
- electrolytes
- later, full haematological and biochemical analysis
Once the baseline bloods have been collected, fluid resuscitation should start immediately.
How much, how fast?

How much fluid should you deliver, and how fast? My “go to” fluid is crystalloids and I generally start with a 20ml/kg bolus of an alkalinising crystalloid.
I perform bolus therapy, so 10ml/kg to 20ml/kg fluid doses rather than shock rates 90ml/kg/hr, as I feel it allows me to better titrate my fluid therapy to effect. It also helps minimise excessive fluid administration and the problems with haemodilution – such as anaemia, hypoproteinaemia and prolonged coagulation times.
As fluids are being delivered, I administer pain relief and start gastric decompression (covered next week).
The decision to administer more fluids depends on whether I have achieved some end point resuscitation variables, such as:
- a reduction in heart rate
- a reduction in capillary refill time
- an improvement of mucus membrane colour
- improvement in pulse pressures
Improvement in mentation is not often reliable as the sedative effect of analgesia, which I generally give during fluid resuscitation, often confounds this effect.
Shock therapy
If evidence of shock still exists, despite the initial fluid boluses and gastric decompression, I will consider more fluids. This can include hypertonic saline or colloids.
In my experience, a repeat of a smaller dose of crystalloid fluid bolus is often adequate (10ml/kg). The transition on to hypertonic saline (7% solution) or colloids is influenced by the results of the aforementioned baseline diagnostics.
A reduction in PCV/total protein suggests blood loss. In this case, I will consider either hypertonic saline (3ml/kg to 5ml/kg of 7% solution), a dose of colloids or even blood products, such as whole blood or packed red blood cells.
If significant prolongation in activated clotting time occurs, likely from consumption, then I may incorporate fresh frozen plasma into my fluid therapy. This is in anticipation of possible surgery, where prolonged coagulation times can not only be troublesome, but life-threatening.
Lactate
A quick note on lactate – I don’t use the baseline reading as a prognostic indicator or an indicator of gastric necrosis. This is supported by recent findings claiming it is not the level of lactate that is predictive, but the degree of improvement in response to fluid resuscitation and gastric decompression.
I have seen unreadable lactate levels – greater than 15mmol/L – in patients who returned to reasonably normal levels within an hour of stabilising. These patients also went on to survive surgery.
Pain relief
After starting IV fluid resuscitation, I generally administer pain relief while the team is preparing for gastric decompression. To keep things simple, I stick to an easily accessible pure opioid agonist at 0.2mg/kg IV. I avoid subcutaneous or even intramuscular administration as the patient is often in shock; the peripheral blood is shunted centrally to the heart and the brain and absorption can be variable.
I find this offers a reliable and great degree of pain relief that helps reduce anxiety levels and, consequently, reduces oxygen demand. It has minimal cardiovascular effects and the mild sedative effect also helps with the process of decompression.
>>> Read Focus on GDV, part 2: Releasing the pressure (gastric decompression)