The amount of sodium required to increase serum sodium concentration to a desired value can be calculated from the following formula:
Sodium deficit = 0.6 × bodyweight (kg) × (normal sodium [mEq/L] – patient sodium [mEq/L])
| Table 1. Sodium content of various fluids | |
|---|---|
| Fluid Type | Sodium content (mEq/L) |
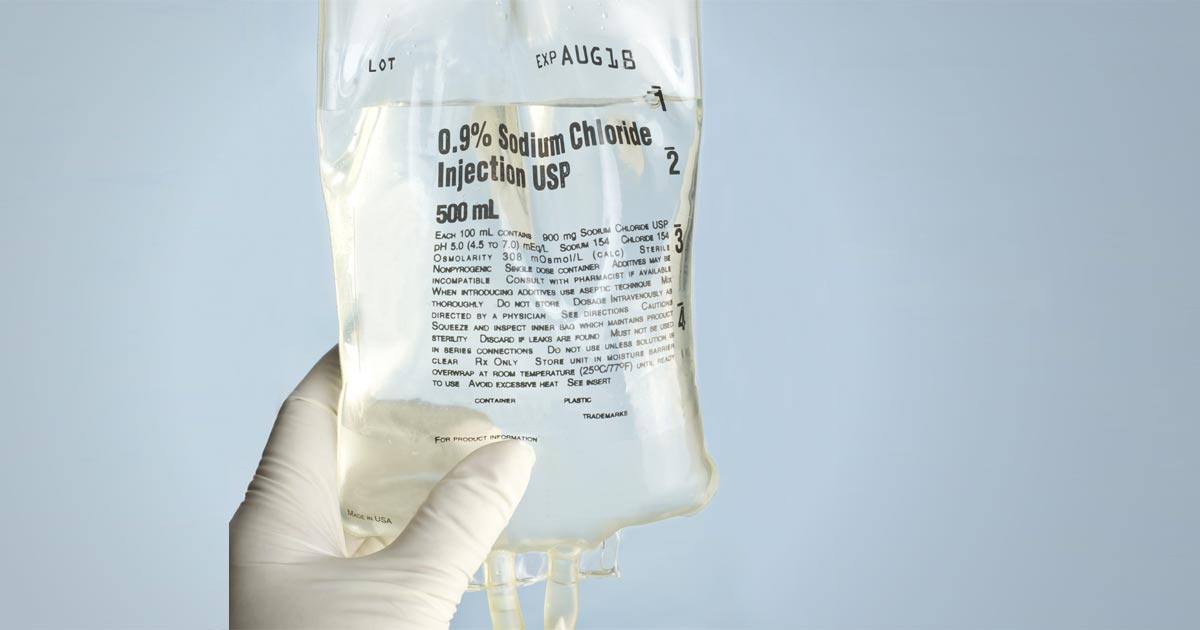
| 0.9% sodium chloride | 154 |
| Normosol-R | 140 |
| Hartmann’s solution |
130 |
| 3% sodium chloride | 513 |
| 7.5% sodium chloride | 1,300 |
This sodium deficit is then replaced over “x” hours, at an average rate of 0.5mEq/L/hr.
In hypovolaemic hyponatraemia patients – where the fluid deficits also need correcting – it is important to select a fluid where the sodium concentration is within 5mEq/L to 10mEq/L of the patient plasma sodium level.
Table 1 shows the sodium content of various fluids. If none of the fluids listed in Table 1 are suitable – for example, the patient’s sodium level is 110 – you can make your own fluid by mixing 5% dextrose in water using the formula below:
Volume of 5% dextrose in water to be added (ml) =
([current IV fluid Na+] – [desired IV fluid Na+]) × 1,000ml ÷ ([desired IV fluid Na+] – [supplemental IV fluid Na+])
Hartmann’s example
The most common cause of severe hyponatraemia is hypoadrenocorticism. Using an example of a severe hyponatraemia of 110mEq/L, I select Hartmann’s solution first, as it has the lowest sodium concentration. How low I dilute Hartmann’s depends on the patient’s volume status.
If the patient requires fluid resuscitation because it is showing signs of poor perfusion – such as elevated heart rate, poor pulse quality, pale gums, prolonged capillary refill time, dull mentation, low core body temperature and elevated lactate – I aim for a sodium concentration the same as the patient. For this example, I would dilute the Hartmann’s to 110mEq/L, as then I can bolus therapy this without elevating the patient’s sodium concentration.
So, aiming for 110mEq/L, the volume of 5% dextrose in water (D5W) required to dilute Hartmann’s is:
= ([130 – 110] × 1,000) ÷ (110 – 0)
= (20 × 1,000) ÷ 110
= 181ml of D5W.
This volume may not fit in the bag, so I remove 150ml from the Hartmann’s bag first and insert 850ml into the equation:
= ([130 – 110] × 850) ÷ (110 – 0)
= (20 × 850) ÷ 110
= 154ml of D5W to be added to the bag for a total volume of 1,054ml with a sodium concentration of 110mEq/L.
Electrolytes can be used on custom solutions to check the final sodium concentration. It will be a couple of mEq/L above or below, due to variations in each Hartmann’s bag.
I bolus with this 110mEq/L of custom solution for correct perfusion, reassess the patient and sodium concentration – and make a solution between 5mEq/L and 10mEq/L higher – and administer at much slower rates with repeated monitoring.
The treatment of hypervolaemic hyponatraemic patients will not be discussed here, as it revolves around treating the underlying medical condition.
Conclusion
Hyponatraemia is a common and potentially life-threatening change in our critical patients.
It is crucial to establish whether this is an acute or chronic change, to avoid development of osmotic demyelination syndrome. If I have any doubt about the timeline, I treat as a chronic change and increase slowly.