Last week we covered haemolysed samples – this week we’re looking at lipaemic samples.
Lipaemic samples are caused by an excess of lipoproteins in the blood, creating a milky/turbid appearance that interferes with multiple biochemical tests and can even cause haemolysis of red blood cells.
Lipaemia can follow recent ingestion of a meal – especially one high in fat. Although not pathognomonic for any diseases, its presence can help increase the suspicion of certain diseases, including:
- pancreatitis
- diabetes mellitus
- hypothyroidism
- hyperadrenocorticism
- primary hyperlipidaemia (in some specific breeds, such as the miniature schnauzer)
It warrants further investigation in patients that have been ill and inappetent.
Irksome interpretations
Lipaemia can dramatically impact laboratory testing and is often troublesome in critically ill patients, making interpretation of biochemistry particularly difficult, if not impossible.
Lipaemia can affect different analysers in different ways, most commonly causing:
- Falsely increased calcium, phosphorus, bilirubin, glucose and total protein (via refractometer) and some liver parameters such as alkaline phosphatase, alanine aminotransferase, aspartate aminotransferase, haemoglobin concentration, and mean corpuscular haemoglobin concentration.
- Falsely decreased sodium, potassium, chloride, albumin and bicarbonate.
Tube tips
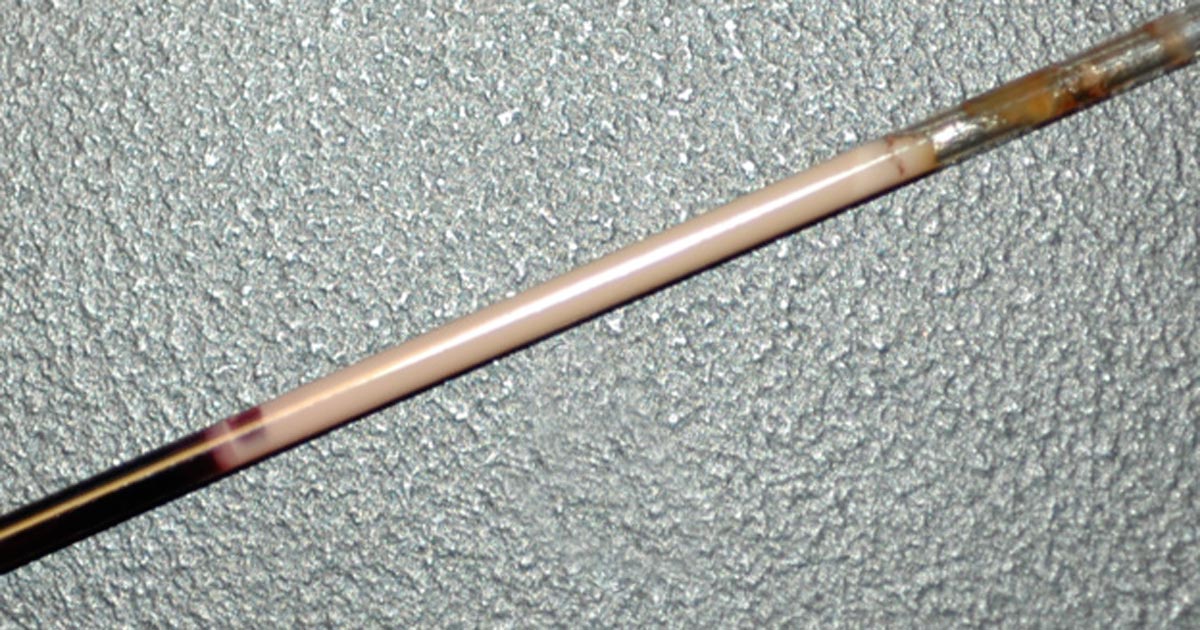
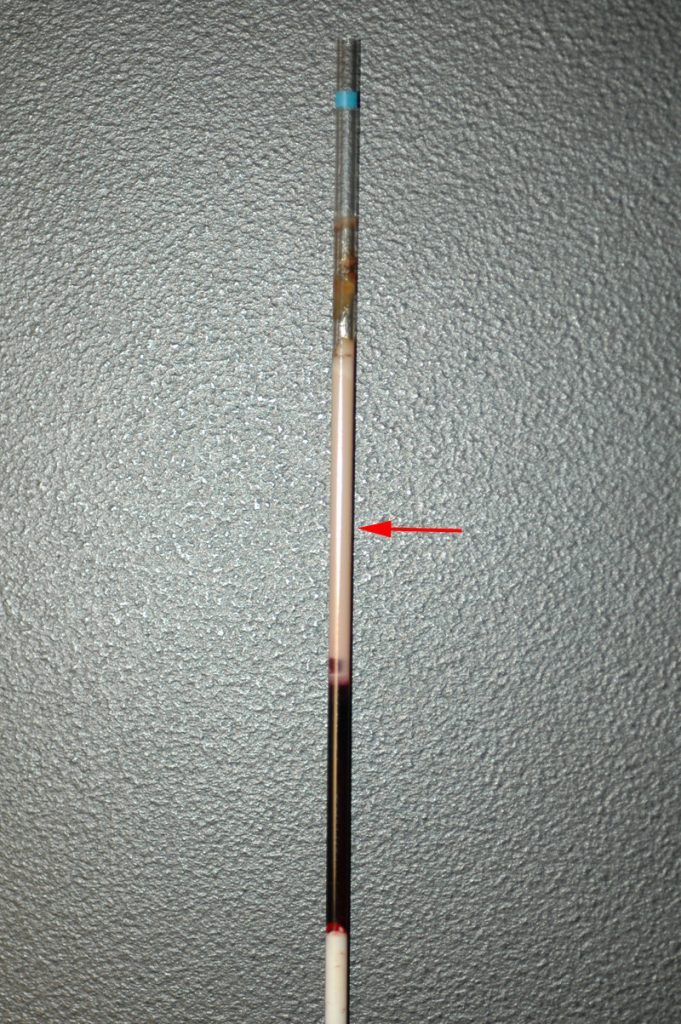
Assessment of a centrifuged haematocrit tube before running a biochemistry panel can help reduce wasted biochemistry consumables.
If the sample is lipaemic in the haematocrit tube then maybe try some of the following tips.
- If blood tests are planned in advance, try fasting the patient beforehand for 12 to 24 hours.
- Repeat sampling a couple of hours later may yield a less lipaemic sample.
- Collecting and centrifuging a larger amount of blood (3ml to 5ml, for example) can sometimes yield enough clear sample between the lipid layer and red blood cells.
- Refrigeration of the sample can help the separation.
- Extract lipids using polar solvents, such as polyethylene glycol.
- Centrifugation at higher than normal speeds (if possible) can also assist in clearing the layer.