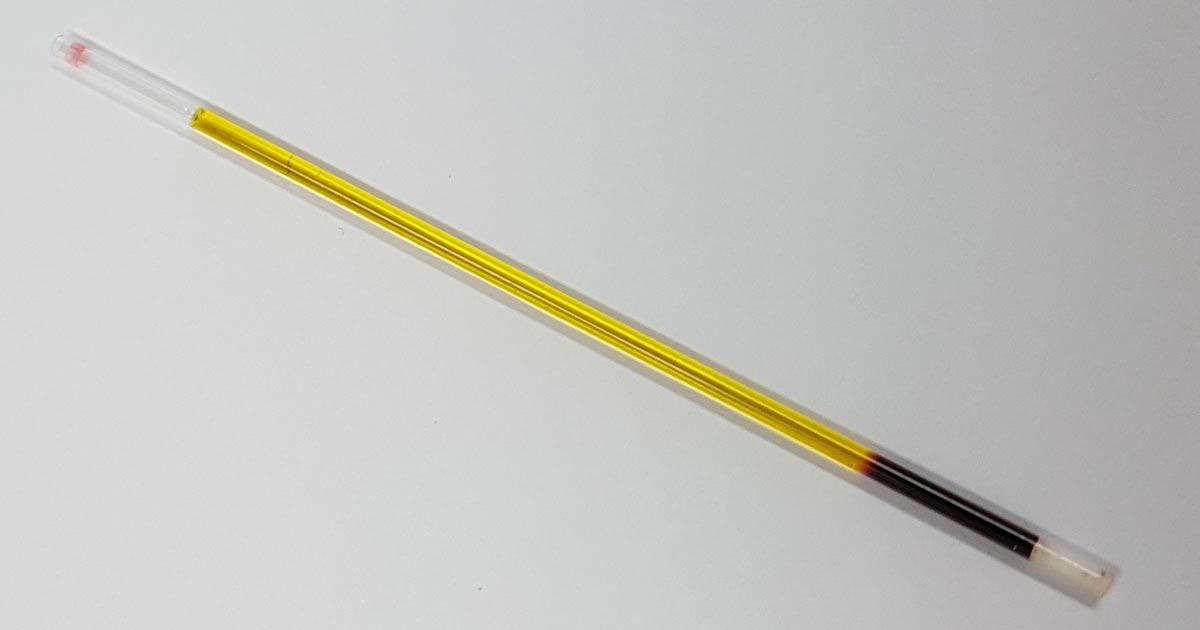
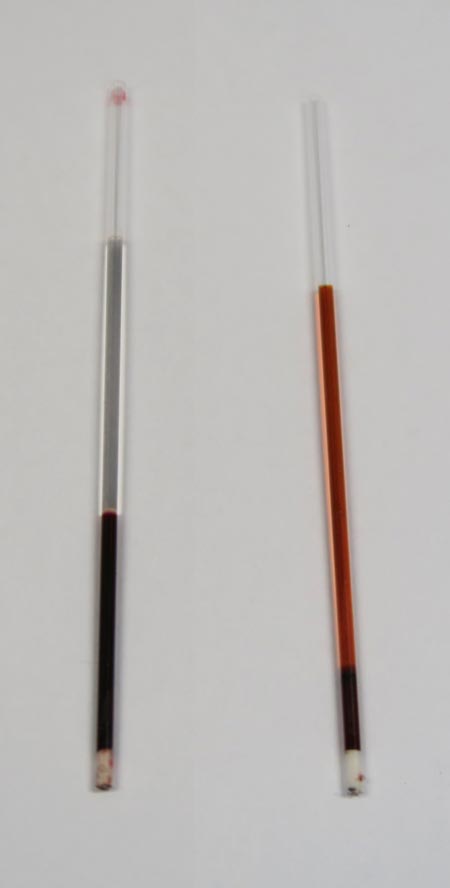
The final discolouration of the serum we are going to cover is icteric serum.
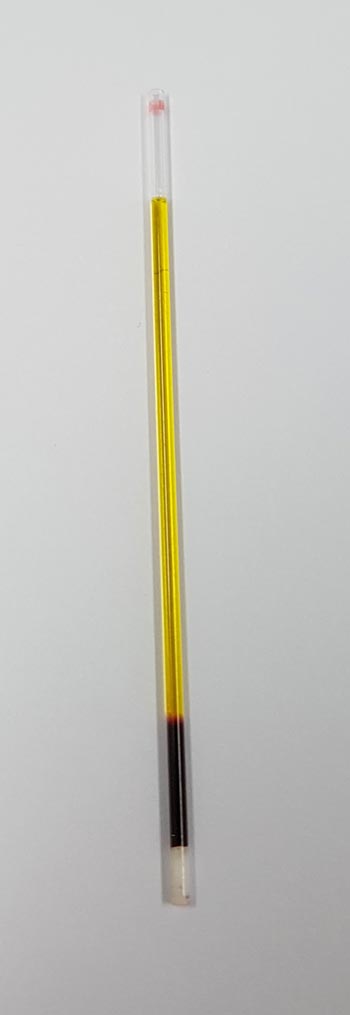
Icteric serum is caused by the presence of excess bilirubin in the blood stream as a result of increased production (pre-hepatic) or inappropriate excretion (hepatic and post-hepatic).
The most common cause of pre-hepatic icterus is haemolytic anaemia, while hepatic disease and biliary tract obstruction are the most common causes for hepatic and post-hepatic icterus, respectively.
Tips on where to start
If icterus and concurrent anaemia exist, my first suspicion would be some kind of pre-hepatic cause. The most common causes are immune-mediated haemolytic anaemia and infectious haemolytic anaemia, such as haemotropic mycoplasma and babesiosis.
Other causes can include snake envenomation and oxidative injury from heavy metal toxicity or onion ingestion.
Regarding hepatic and post-hepatic causes, unfortunately it is not always clear-cut. Both are commonly associated with elevation in both alanine transaminase (ALT) and alkaline phosphatase (ALKP), and, although no specific changes are pathognomonic for hepatic or post-hepatic disease, the pattern of change may help identify the origin of the cause. ALT is released from the inside of hepatocytes, and in higher amounts when cell damage occurs.
Hepatic hints
Some pointers on what you can do to help differentiate:
- Compare the ALT and ALKP elevation; if one is in order of magnitudes higher than the other then it can help point to an origin.
- If the cause is of hepatic origin, one would expect the ALT to be significantly more elevated than the ALPK. Likewise, this is usually true in reverse for post-hepatic causes. However, it should be noted in chronic hepatic diseases, where active damage to hepatocytes is comparatively lower, a mild increase in ALT and marked increase in ALPK does not preclude disease of hepatic origin. Therefore, biopsies should always be used for definitive diagnosis.
- If other biochemistry parameters such as albumin, glucose and cholesterol are low, or prolonged clotting times are present, the case for a hepatic origin is strengthened.
- The gallbladder and bile duct can be assessed using abdominal ultrasonography. The presence of a dilated bile duct, or evidence supportive of pancreatitis, is highly suggestive of a post-hepatic cause.
Finally, it is important to be aware of the impact on hyperbilirubinaemia on laboratory testing. Hyperbilirubinaemia generally causes decreased cholesterol, triglyceride, creatinine, lipase, total protein and gamma-glutamyltransferase levels.