Anaesthetic complications occur frequently, but are rarely fatal. The majority of those can be anticipated, if not avoided, with an accurate assessment of the patient and adequate preoperative stabilisation. Some anaesthetic complications are secondary to the drugs used in the perioperative period, while others are a direct consequence of the patient’s underlying condition. Hypoventilation, hypothermia and hypotension are the most common complications that occur during anaesthetic and, if not treated appropriately, can became emergencies and significantly affect the outcome.
“Anaesthesia is 99% boredom and 1% panic”. This adage tries to capture the idea that, most of the time, anaesthesia is routine and predictable, but when an emergency happens, the progression to a critical state can be rapid and difficult to control.
This article discusses some of the more common anaesthetic complications and how to deal with them. However, two other factors should be considered by all of the clinical team members about to embark on anaesthetising a patient: preanaesthetic assessment of the patient to identify any pathological or physiological abnormalities that may affect the procedure; and preanaesthetic assessment of the environment.
This second aspect, often described as a “pre-flight checklist”, is analogous to a pilot checking the aeroplane (and him or herself) prior to take-off, and should consider elements such as the anaesthetic machine, team members, the planned procedure, predicted adverse events (such as aspiration or haemorrhage) and steps taken to prevent or deal with them1.
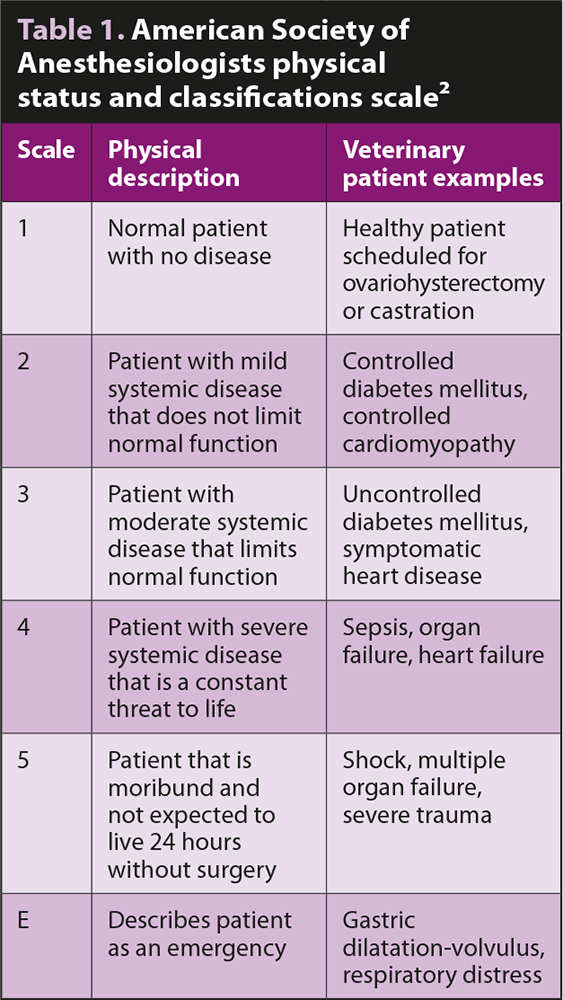
In-depth assessment of patients before anaesthetic is a cornerstone in prevention of any anaesthetic complication. Using the scale developed by the American Society of Anesthesiologists (ASA) is helpful to identify patients at risk. Animals are graded from 1 to 5 – depending on the severity of their disease (Table 1). It has been shown that risk of death during anaesthesia in healthy patients (ASA 1 to 2) was 0.05% for dogs and 0.11% for cats, increasing up to 1.33% for dogs and 1.40% for cats in ill patients (ASA 3 to 5)3.
Even if the death rate is relatively low in our patients, anaesthetic complications occur frequently. In a group of 1,281 dogs, hypoventilation, hypothermia and hypotension occurred in 63%, 53% and 38% of patients respectively4.
The following is a list of the most common anaesthetic complications and emergencies, with some guidance on how to deal with them.
Hypoventilation
Hypoventilation is defined as an increase in end-tidal CO2 or partial pressure of CO2 (PCO2; above 45mmHg). It is commonly encountered in sedated or anaesthetised patients, as most anaesthetic drugs directly affect the brainstem respiratory centres, causing a degree of respiratory depression5. While mild hypercapnia can be tolerated (permissive hypercapnia), a sustained and significant increase in CO2 should prompt intervention as severe respiratory acidosis can directly depress cardiac and vascular muscle, and can cause arrhythmias and depression of the CNS.
In this case:
- Provide oxygen and intubate if needed.
- Consider reducing/reversing anaesthetic drugs.
- Check the anaesthetic machine and endotracheal (ET) tube to make sure it is set up properly and that no malfunctions exist (such as oxygen flow, kinking of the ET tube or blockage with secretions, accidental intubation of the oesophagus, rather than the trachea).
- Consider intermittent positive pressure ventilation (IPPV).
- Check patient temperature as hypothermia inhibits the respiratory centres.
Hypoxaemia
Hypoxaemia occurs when arterial partial pressure of oxygen (PaO2) is less than 80mmHg or arterial blood haemoglobin saturation (SaO2) is less than 95%6. If hypoxia is identified, the first thing to do is supplement oxygen via flow by mask, nasal prongs and intubate if needed.
If the patient is already intubated and breathing 100% oxygen (fraction of inspired oxygen [FIO2] 1.0) then:
- Check the anaesthetic machine and ET tube to make sure it is set up properly and no malfunctions exist (see hypoventilation before).
- Auscultate the patient on both hemithoraces to rule out bronchial intubation or pleural space disease. Re-intubate if needed.
- Check CO2 and treat hypoventilation if present. Consider IPPV.
- If the animal is already receiving IPPV, increase positive end-expiratory pressure or perform recruitment manoeuvres.
- Consider pre-existent or iatrogenic pleural space disease (pleural effusion versus pneumothorax) – consider point-of-care ultrasound to rule these out.
- Ensure adequate perfusion.
Hypothermia
Hypothermia occurs due to a combination of cold hospital environment and altered patient thermoregulation. While hypothermia protects against ischaemia and hypoxia, a reduction of core body temperature is also associated with vasoconstriction, lactic acidosis, reduced drug metabolism, impaired coagulation and impaired immune system7. Forced air warming systems are an effective means of preserving and increasing body heat in the anaesthetised patient8, while humidification and warming of inhaled gas have been shown to be ineffective as a sole means of maintaining core temperature in companion animals9.
Hypotension
Many factors are associated with the development of hypotension, including most anaesthetic agents, hypovolaemia, haemorrhage, peripheral vasodilation and myocardial dysfunction5. If a patient is hypotensive consider:
- Anaesthetic level and anaesthetic drug. General anaesthetics cause changes in cardiac function, vascular reactivity and cardiovascular reflexes, and significantly alter distribution of cardiac output to various organs10. Decreasing the depth of anaesthesia can be enough to treat hypotension.
- Hypovolaemia. Secondary to antecedent losses (haemorrhage, vomiting, diarrhoea, third space losses) not adequately corrected before induction or excessive intraoperative losses (for example, haemorrhage). A fluid bolus with isotonic crystalloids (10ml/kg to 20ml/kg), colloids (2ml/kg to 5ml/kg) or administration of blood products (packed red blood cells if haemorrhage is identified, fresh frozen plasma if concurrent coagulopathy is present) can be administered to correct hypovolaemia.
- Vasodilation. This can be secondary to the anaesthetic drugs or underlying condition, such as systemic inflammatory response syndrome, sepsis or anaphylaxis. In euvolaemic patients consider administration of vasoactive agents, such as norepinephrine, vasopressin, ephedrine, dopamine or epinephrine.
- Reduced cardiac contractility. This can be secondary to anaesthetic drugs or underlying conditions (for example, sepsis and dilated cardiomyopathy). Preanaesthetic assessment will help identify patients at risk. Drugs with positive inotropic function to treat this include dobutamine, pimobendan, dopamine, or epinephrine.
Cardiac dysrhythmias
Cardiac dysrhythmias can occur as a result of pre-existing medical conditions or as a response to surgery and anaesthesia. Most of them have little clinical significance and do not require treatment; however, if perfusion is compromised, immediate treatment is needed.
When a bradyarrhythmia is identified consider:
- High vagal tone. This will usually be a sinus bradycardia, although atrioventricular block can sometimes be present and can be breed-related or caused by an underlying medical condition or pain (for example, manipulation of viscera during abdominal surgery or oculo-vagal reflex). If the bradyarrhythmia is severe (lower than 40bpm), it can be treated with glycopyrrolate or atropine (atropine has a faster onset, therefore is the drug of choice in life-threatening situations).
- Hypothermia. This results in decreased depolarisation of cardiac pacemaker cells, causing bradycardia. Since this bradycardia is not vagally mediated it can be refractory to standard therapies such as atropine.
- Electrolytes. Severe hyperkalaemia, more commonly, or hypokalaemia can cause bradycardia. It usually appears as atrial standstill on the electrocardiogram (ECG).
- Increased intracranial pressure. Sinus bradycardia is secondary to elevated arterial blood pressure. Treatments of choice are hypertonic saline and mannitol.
- Anaesthetic drugs. Medetomidine and dexmedetomidine can cause sinus bradycardia and atrioventricular blocks11,12; in this case atipamezole should be the first-line treatment before atropine to reduce the risk of dysrhythmia. Marked bradycardia associated with opioid use13,14 should be treated with naloxone, although it should be remembered this drug will also reverse the analgesic effects of the opioid.
If a tachyarrhythmia is present consider:
- Pain or inadequate anaesthetic level. A sinus tachycardia – usually associated with moderate hypertension – is a hallmark of pain. Review the analgesic and anaesthetic plan and adjust accordingly.
- Compensatory tachycardia. Hypotension, hypoxia, hypercapnia and hypokalaemia can induce a reflex tachycardia. Correcting these derangements will also treat the tachycardia.
- Anaesthetic drugs. Atropine and glycopyrrolate cause sinus tachycardia while thiopental and ketamine increase the likelihood of norepinephrine-induced dysrhythmias during halothane and isoflurane anaesthesia15,16.
- Underlying medical condition. Gastric dilatation-volvulus17, splenic disease18, cardiac trauma19 and all causes of hypoxia are associated with ventricular premature complexes and ventricular tachycardia. If treatment is indicated (heart rate above 160bpm to 180bpm, hypotension, malignant dysrhythmias), lidocaine is the first-line treatment. Procainamide or amiodarone are second-line agents in refractory ventricular tachycardias.
- Ventricular fibrillation. This requires cardiopulmonary resuscitation (CPR) and defibrillation.
Hypersensitivity reactions
Hypersensitivity reactions can occur in the peri-anaesthetic period and can be life-threatening. The two most common types are anaphylactic reactions (antigen-immune complex mediated or type 1), which require a previous exposure to the agent, and anaphylactoid reactions, which do not involve IgE and do not require previous sensitisation20. They cannot be clinically distinguished and can be equally dangerous. Hypotension, tachycardia, arrhythmias, pulmonary and portal hypertension, and cutaneous changes can occur.
If suspicion of a severe allergic reaction exists:
- Discontinue all drug administration.
- Administer oxygen – intubate the patient if needed.
- Administer adrenaline.
- Administer an antihistamine (diphenhydramine or chlorpheniramine).
- Administer a bronchodilator (salbutamol or aminophylline).
- If hypotension is present, administer a bolus of hypertonic crystalloids and consider using a vasopressor.
- No concrete evidence is available to support or oppose the use of corticosteroids in emergency management of anaphylaxis.
Cardiopulmonary arrest
Cardiopulmonary arrest (CPA) occurs as a result of the cessation of ventilation and circulation. When CPA is suspected, administration of all anaesthetic drugs should be suspended and drugs previously administered should be reversed. Basic life support needs to be started immediately as any delay significantly reduces the chances of return to spontaneous circulation (ROSC).
Basic life support
Basic life support (BLS) consists of administrating chest compressions and ventilation. The optimal compression rate is 100 to 120 per minute.
Compressions can be performed:
- Over the widest portion of the chest to maximally employ the thoracic pump theory. This is valid for most dogs.
- With the hands directly over the heart to employ the cardiac pump theory. This is useful in keel-chested dogs such as greyhounds, and small (less than 7kg) dogs and cats.
- On the sternum, directly over the heart with the patient in dorsal recumbency, in barrel-chested dogs such as English bulldogs.
In cases of tension pneumothorax, pleural or pericardial effusions, or significant chest wall/diaphragm injuries, open-chest CPR should be performed.
Airways should be secured with orotracheal intubation and oxygen should be delivered with a FIO2 of 1.0. Optimal ventilation rate is 10 breaths per minute with a tidal volume of 10ml/kg. Compressions should not be stopped during ventilation.
BLS should be administered in two-minute cycles. The operator delivering the compressions should be changed at every cycle to avoid fatigue and ineffective compressions. At the end of every BLS cycle, the team leader should look for signs of ROSC (ECG, pulse, apex beat, increase in end-tidal CO2). Both during ROSC checks and swapping of compressor, delays in administrating chest compressions should be minimised.
Advanced life support
Advanced life support includes therapy with vasopressors, positive inotropes and anticholinergics, correction of electrolyte/acid-base disturbances, volume deficits and defibrillation. The two drugs routinely used during cardiopulmonary resuscitation are epinephrine and atropine. Epinephrine is a non-specific adrenergic agonist used for its vasopressor (α1) activity. The initial dose is 0.01mg/kg and it should be administered every three to five minutes (every other BLS cycle). Atropine is a parasympathetic antagonist. The literature has not shown beneficial or detrimental effect of its use at standard dosing (0.04mg/kg) during CPR. Its action lasts up to 20 minutes.
Monitoring
During CPR, minimum monitoring includes ECG and capnography. ECG is needed to recognise “shockable” rhythms (ventricular fibrillation and pulseless ventricular tachycardia), while capnography is useful to assess the quality of CPR: an end-tidal CO2 above 15mmHg in dogs and 20mmHg in cats is associated with effective CPR and an increased rate of ROSC.
Consensus guidelines, printable CPR algorithms and CPR drug charts can be found in the open access Reassessment Campaign on Veterinary Resuscitation guidelines21.
- Note some drugs in this article are used under the cascade.

Leave a Reply