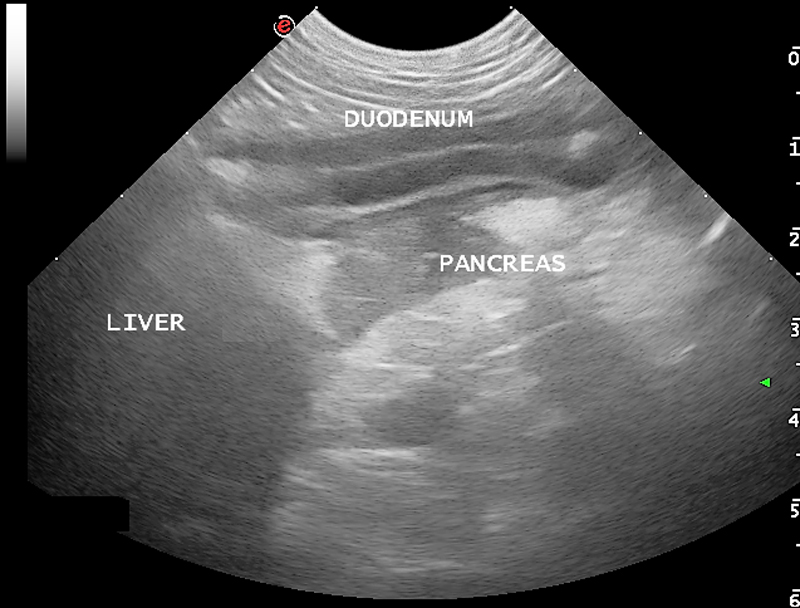
Last week we covered diagnosing pancreatitis and the challenges associated with doing so. This week we look at management.
The treatment of pancreatitis largely involves supportive care and monitoring for potential complications. Here, we recap the fundamentals.
IV fluids
IV fluids are critical in the acute phase to restore perfusion to core organs and correct hydration deficits. Once achieved, the goal is then to cover maintenance requirements and ongoing losses.
Hypoproteinemia can develop due to a combination of haemodilution, increased losses in to inflammatory exudates or into gastrointestinal tract, and decreased production due to reduced intake.
Colloidal therapy or plasma can be considered, but enteral nutrition is more effective and has numerous other benefits.
Pain relief
Pain relief largely involves the use of opioids.
Pure opioid agonists, such as methadone, fentanyl constant rate infusions (CRIs) or fentanyl patches, are most commonly seen in dogs. In cats, partial agonists, such as buprenorphine, are favoured as the condition is generally less painful compared to dogs.
NSAIDs should be avoided due to concerns of poor perfusion, concurrent kidney and gastrointestinal involvement.
Antiemetic therapy
Metoclopromide CRI and maropitant are the mainstays. Antacids, such as esomeprozole, are included to help reduce the risk of gastric ulceration from stress.
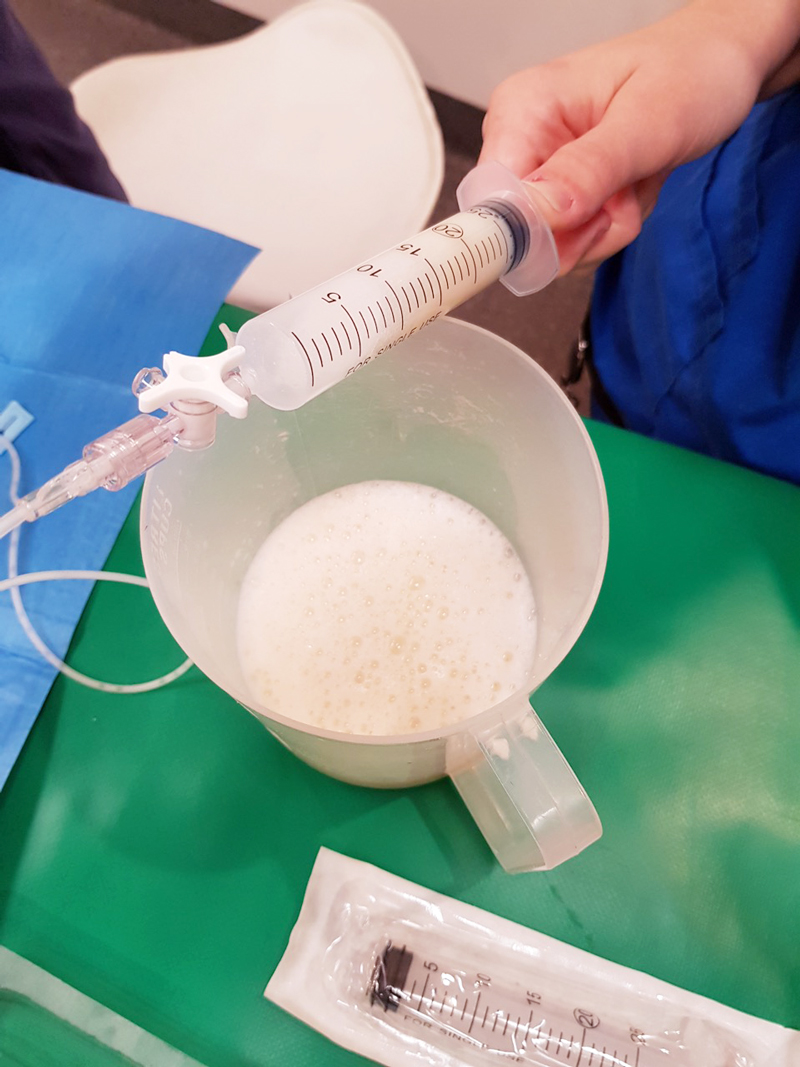
Early enteral nutrition
Numerous studies have demonstrated the benefit of early enteral nutrition and patients should be encouraged to eat a low-fat diet as soon as possible. Enteral nutrition has been shown to be more beneficial than withholding food as it reduces recovery times and helps maintain enterocyte health.
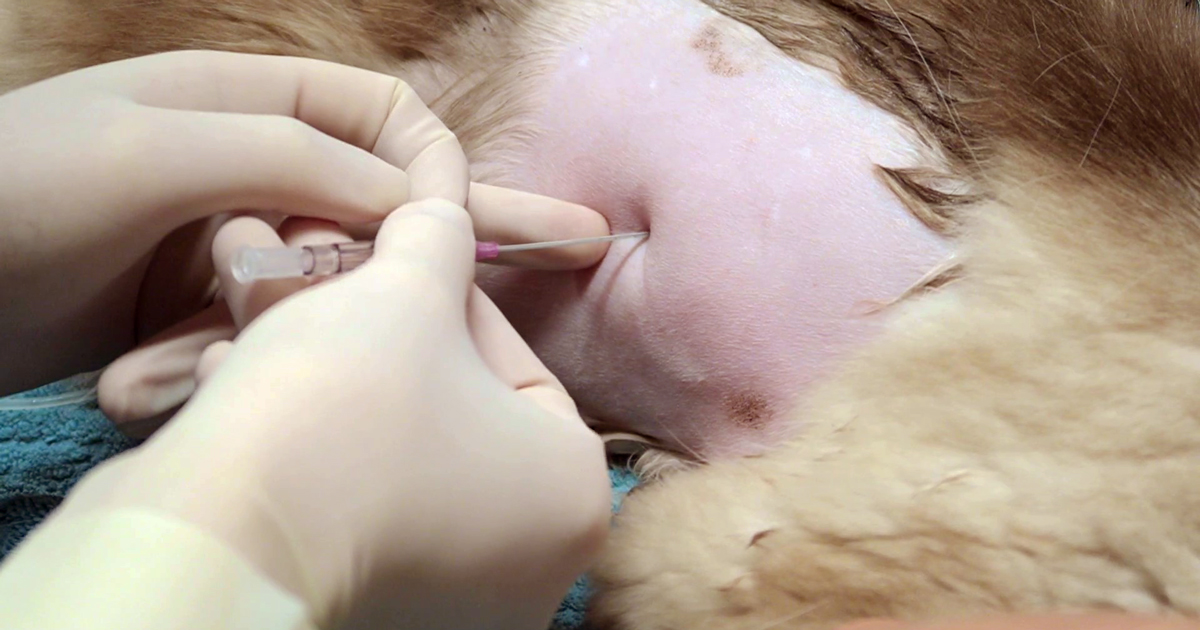
If there has been a protracted period of anorexia then a nasogastric or nasoesophageal tube should be placed. A nasoesophageal tube has the added benefit of allowing excessive gastric secretions to be suctioned, as well as for feeding. Due the chronic nature of the disease in cats, oesophagostomy tubes are often placed so that nutritional support can be delivery for prolonged periods of time.
Antibiotics
Antibiotics are generally not indicated in canine pancreatitis unless markers of sepsis or if a septic exudate are found (this is an indication for exploratory surgery). In which case, triple antibiotic therapy consisting most commonly of amoxicillin, enrofloxacin and metronidazole are indicated.
It has been reported 35% of feline pancreatitis patients have bacterial infections; therefore, antibiotics are often included in the treatment of feline pancreatitis.
Exploratory laparotomy
This is indicated when the following has occurred:
- Extra-hepatic biliary obstruction that does not resolve with medical management.
- Septic abdomen (as mentioned above).
- Pancreatic abscessation.
Prognosis
The prognosis for pancreatitis is variable and dependent on the severity of the disease.
In mild to moderate canine pancreatitis (which is the most common), the prognosis is generally good as they will normally respond well to supportive therapy and resolution of clinical signs occurs within several days of initiating treatment. However, with severe acute, necrotising pancreatitis, the prognosis is guarded as it can progress into systemic inflammatory response syndrome, disseminated intravascular coagulation and multiple organ failure – which has a high mortality rate.
The prognosis of acute feline pancreatitis is generally guarded due to the chronic nature of the disease and the propensity to involve multiple organ systems.