We spend five years at vet school learning a myriad of vet jargon; a whole new language, with a fair bit of Latin thrown in too.
When you think about it, even the “simple” descriptive and directional words – e.g. caudal/cranial – were alien to us before vet school. The funny thing is, just as you become fluent in vet-speak, you have to be able to translate this back to English for clients.
I used to listen to vets converse with clients while on EMS placements, and could easily pick out those who communicated better. When witnessing those who weren’t so good at translating, I swore to myself I would never befuddle a client with medical words – surely it’s not that difficult to explain things in simple terms?
Slipping

While having a non-vet family and boyfriend has helped keep me “bilingual”, I fear I am starting to fall into the jargon trap already.
The first sign appeared when in conversation with the aforementioned better half who, while not in the profession, has grasped a fair idea of the vet world after some years by my side.
After listening to one of my many ramblings about vet life, he asked “what is a mucosa?” and I suddenly realised I was possibly losing my ability to communicate like a normal human being.
Meanwhile, I have found myself on more than one occasion having a complete mental block when trying to think of the “normal” word for something, with the technical term holding strongest in my mind. But I guess that comes with experience, and explaining things to different clients in time.
Beneath the surface
The way vets communicate with each other is important too – while the language we use can seem subtle, it can have deeper meanings.
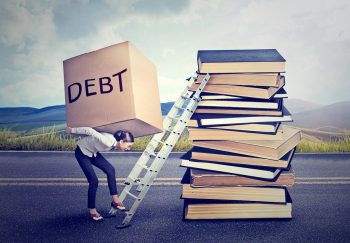
One particular word I fear is becoming normalised within our profession is not a medical word at all – “survive” (and the derivatives thereof). New grads may joke about having “survived” X number of months in practice, and when asked “how are you getting on?”, “surviving” is all too common an answer. Throwing this word around makes it seem as though it loses meaning, but I think it actually has the opposite effect.
The Oxford Dictionary meaning of “survive” is to “continue to live or exist, especially in spite of danger or hardship.” And we relate this to the veterinary world all the time.
Justification?
The all too frequent use of the word either suggests we are in a constant state of hardship – be that emotional, physical, mental or financial – or that we are exaggerating.

Justified or not, I think we use the word too often; we shouldn’t be merely “surviving” – we all worked hard to enter this profession, and nobody said being a new grad would be easy – but it doesn’t need to be horrific.
If you feel like you’re coasting along, just about surviving, talk to your friends, colleagues, an independent ear – get some advice to find out either how to get more on top of things, or whether you’re truly in the right kind of practice environment for you.
And if you’re more than surviving, stop brandishing the word about carelessly for the sake of those who feel they’re just about keeping their heads above water. The language you use is more important than you may realise.